Understanding Menstrual Digestive Symptoms
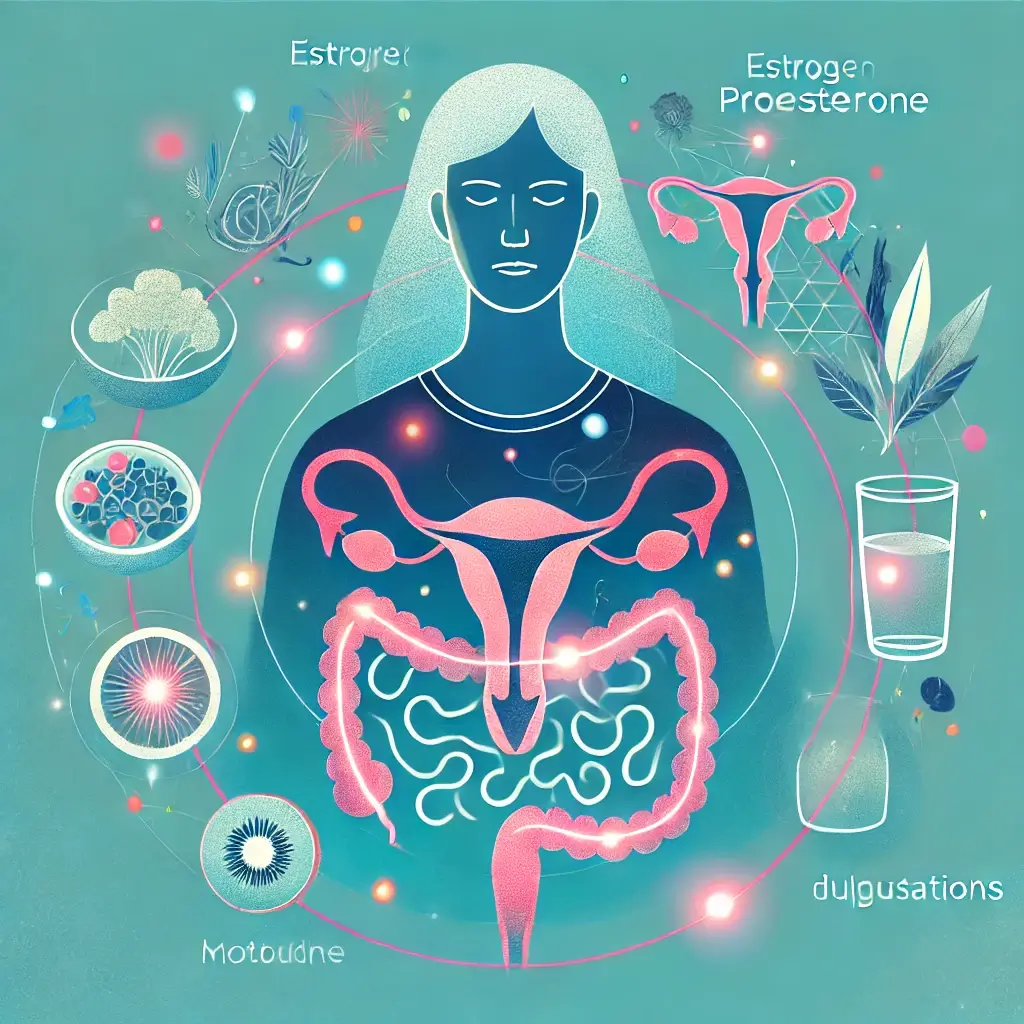
For many women, menstruation brings a mix of physical and emotional symptoms. While cramps, bloating, and mood swings are frequently discussed, digestive issues during menstruation often go unnoticed. Constipation, diarrhea, and excessive gas are common companions to menstrual discomfort, complicating daily activities and overall well-being. Despite their frequency, the connection between menstrual hormones and digestion remains underexplored in public discourse.
Hormones like estrogen and progesterone, known for their role in regulating the menstrual cycle, also influence digestion. Prostaglandins affecting gut motility, another group of hormone-like molecules, exacerbate these disruptions. These hormonal fluctuations can slow digestion or cause sudden contractions, leading to a wide range of gastrointestinal symptoms.
This article delves into the science behind digestive disturbances during menstruation, shedding light on hormonal interactions, current medical research, and practical strategies to alleviate discomfort. Understanding these mechanisms empowers women to make informed choices about their health and navigate their cycles with greater ease.
The Impact of Hormonal Fluctuations on Digestion
The menstrual cycle is orchestrated by a symphony of hormones, primarily estrogen, progesterone, and prostaglandins. While their primary roles involve preparing the body for potential pregnancy, their influence extends to various other systems, including digestion.
Progesterone’s Role in Gut Motility
Progesterone’s effect on smooth muscle activity rises after ovulation and peaks before menstruation, is known to relax smooth muscles in the body. While this relaxation is beneficial in preventing premature uterine contractions, it also slows down gut motility. Reduced gut motility often leads to constipation, causing bloating, discomfort, and sometimes pain. A 2014 review published in Digestive Diseases and Sciences found that progesterone’s effects on smooth muscle activity contribute significantly to constipation during menstruation (Liu et al., 2014).
Prostaglandins and Gut Contractions
Prostaglandins are hormone-like molecules responsible for triggering uterine contractions to shed the uterine lining during menstruation. Unfortunately, their influence doesn’t stop at the uterus. Prostaglandins affecting intestinal smooth muscles can also affect the smooth muscles in the intestines, leading to diarrhea or increased bowel movements. A 2018 study in Frontiers in Pharmacology highlighted the dual role of prostaglandins in causing menstrual cramps and stimulating gut contractions (Gabor et al., 2018).
Water Retention and Bloating
Hormonal shifts affecting water retention, particularly fluctuating estrogen levels, contribute to water retention. This retention can make the intestines sluggish, further exacerbating constipation and bloating. Many women report feeling heavier and more sluggish in the days leading up to their periods, a sensation closely tied to these hormonal changes.
Managing Digestive Issues During Menstruation
Although hormonal fluctuations are inevitable, adopting specific lifestyle strategies can mitigate their impact on digestion. These steps focus on maintaining gut health and reducing symptom severity during menstruation.
Fiber-Rich Diet
A high-fiber diet for menstrual constipation can alleviate constipation by promoting regular bowel movements. Foods like whole grains, fruits, vegetables, and legumes are excellent sources of fiber. A 2016 study in Nutrients emphasized the role of dietary fiber in improving stool consistency and relieving constipation, particularly during hormonal fluctuations (Liu et al., 2016).
Stay Hydrated
Adequate hydration for digestive health supports digestion and prevents constipation by softening stool. Women should aim to drink at least 8–10 glasses of water daily, particularly during their cycle, to reduce bloating and improve overall gut motility.
Stress Management
Stress can exacerbate digestive issues by triggering the gut-brain axis during menstruation, a bidirectional communication system between the central nervous system and the gastrointestinal system. Techniques such as yoga, meditation, and mindfulness can help reduce stress-related digestive problems.
Limit Bloating Triggers
Foods that contribute to gas and bloating, such as processed snacks, sugary drinks, and cruciferous vegetables, should be consumed in moderation during menstruation. Replacing these with anti-inflammatory foods for menstrual health, like leafy greens and berries, can promote better digestion.
Probiotic Support
Probiotics for menstrual gut health, found in fermented foods or supplements, can help maintain a healthy gut microbiome, potentially reducing bloating and other digestive issues. Consulting a healthcare provider can help determine the best probiotic strains for individual needs.
Heat Therapy
Applying a warm compress to the lower abdomen can relax muscles, ease cramps, and reduce bloating. This simple technique can complement dietary and lifestyle adjustments for added relief.
Beyond the Period: Long-Term Gut Health
Menstrual-related digestive issues often mirror overall gut health. Women can minimize these symptoms by maintaining a healthy lifestyle throughout their cycle. Regular physical activity, a balanced diet, and consistent sleep patterns can promote optimal gut function. Additionally, developing long-term stress management strategies can improve the body’s response to hormonal changes.
Conclusion
Digestive disturbances during menstruation are common yet manageable. By understanding the hormonal connections and adopting targeted strategies, women can alleviate symptoms and enhance their overall quality of life. While most symptoms can be addressed through lifestyle changes, persistent digestive issues during menstruation should be evaluated by a healthcare professional to rule out underlying conditions. A proactive approach to gut health empowers women to navigate their cycles with greater comfort and confidence.
References
Gabor, G. S., Nadeem, A., Laporte, J. R., Munshi, G., Brar, S. S., & Buchanan, E. M. (2018). The role of prostaglandins in women’s health and disease. Frontiers in Pharmacology, 9.
Liu, S., Zheng, H., Hall, L. M., Guo, Z., Wang, Z., … Li, L. (2016). Fiber intake and constipation in a Chinese population. Nutrients.
Liu, Z., & Wang, X. (2014). Hormonal regulation of gut motility. Digestive Diseases and Sciences.