Understanding the Impact of Digestive Health
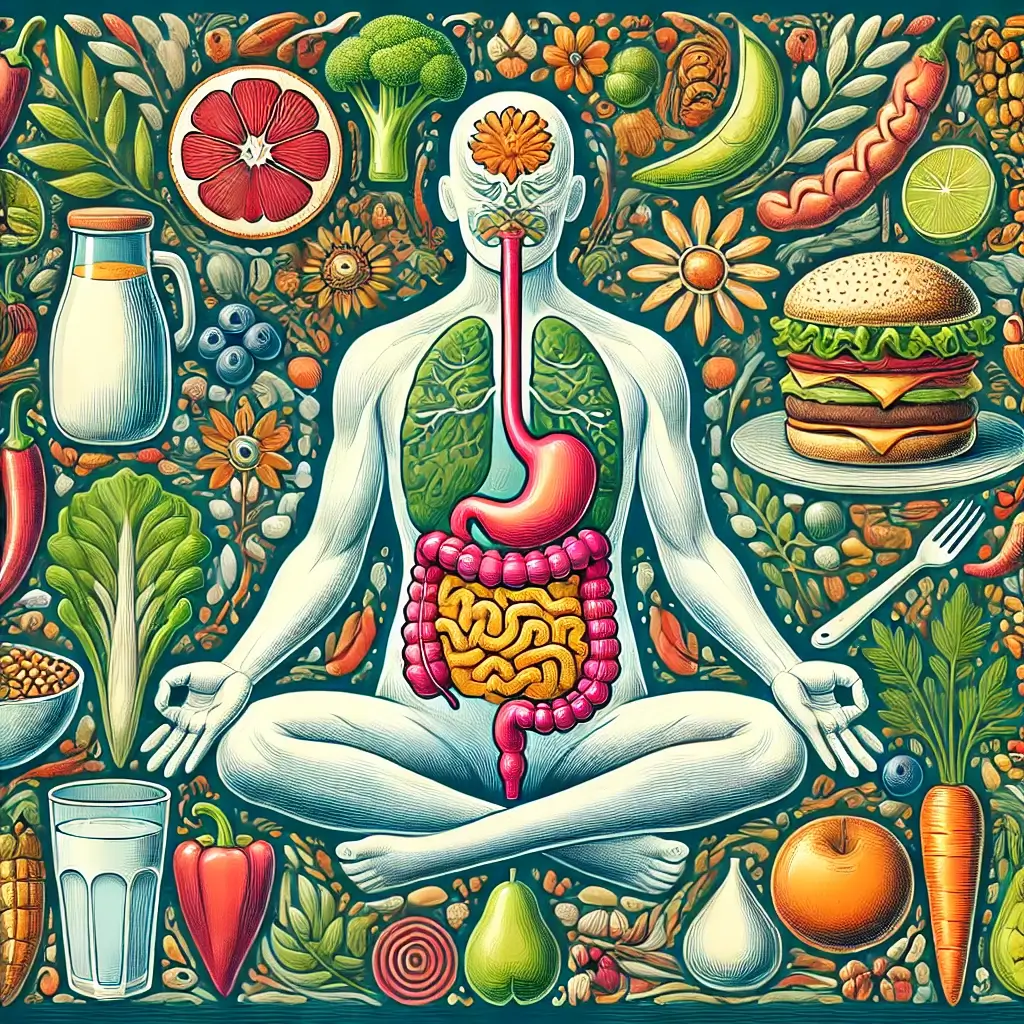
Digestive discomfort is more than a physical nuisance—it can ripple through your life, affecting mental clarity and energy levels. The digestive system, often referred to as the “second brain,” is intricately tied to every system in the body. Gut health influences immune function, hormonal balance, and even mental well-being. Conditions like bloating, gas, heartburn, and diarrhea disrupt daily life for millions, with significant implications for productivity and quality of life.
The Role of Diet in Digestive Health
Fortunately, diet is a controllable factor that can dramatically improve digestive health. Scientific research has identified specific food culprits responsible for triggering or worsening digestive issues. Avoiding these foods and adopting mindful eating practices can ease symptoms and improve gut function. This article will examine how dietary choices influence digestive health, delve into the foods to avoid, and explore practical strategies for building a gut-friendly diet. A holistic approach that incorporates nutrition, stress management, and professional guidance can transform not only digestive health but overall well-being.
Foods to Avoid for Digestive Wellness
FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) are short-chain carbohydrates that ferment in the gut, causing bloating and gas in individuals with sensitive digestive systems. A groundbreaking study in Gastroenterology found that a low-FODMAP diet significantly reduced symptoms of irritable bowel syndrome (IBS) in 75% of participants (Shepherd & Gibson, 2010). Common high-FODMAP foods include:
Fruits: Apples, pears, cherries, watermelon, and dried fruits
Vegetables: Garlic, onions, cauliflower, broccoli, and Brussels sprouts
Dairy Products: Milk, yogurt, and soft cheeses (unless lactose-free)
Sweeteners: Sorbitol, mannitol, and xylitol (found in sugar-free gum and candies)
Eliminating these foods can alleviate symptoms for many individuals. However, reintroducing them one by one under the guidance of a dietitian can help identify personal triggers.
Impact of Spicy Foods on GERD
For individuals with gastroesophageal reflux disease (GERD), spicy foods are a well-known irritant. Capsaicin, the active compound in chili peppers, can weaken the lower esophageal sphincter and cause acid to reflux into the esophagus, triggering heartburn. A study in Digestive Diseases and Sciences confirmed that capsaicin worsens esophageal sensitivity in GERD patients (Zhang et al., 2012).
The Effects of Fatty and Greasy Foods
High-fat meals are another common trigger for digestive discomfort. Fat slows stomach emptying, which can lead to bloating, indigestion, and heartburn. Research also suggests that a high-fat diet can negatively alter gut microbiota, exacerbating inflammation and digestive issues (Murphy et al., 2015).
Understanding Artificial Sweeteners
Artificial sweeteners such as sorbitol, mannitol, and xylitol are popular in sugar-free products. However, these compounds are poorly absorbed in the small intestine, leading to fermentation in the colon and symptoms like gas and diarrhea. A review in Regulatory Toxicology and Pharmacology emphasized the need for moderation when consuming these sweeteners, particularly for individuals with IBS (Magnuson et al., 2016).
Strategies for Digestive Wellness
Mindful Eating: Chewing thoroughly and eating slowly enhances digestion, reducing the likelihood of overeating or indigestion.
Hydration: Drinking plenty of water aids in digestion and prevents constipation by softening stool.
Stress Management: Chronic stress can disrupt gut motility and alter microbiota composition. Incorporating relaxation techniques like yoga or meditation can support overall gut health.
Gut-Friendly Foods: Prioritize low-FODMAP vegetables, lean proteins, and whole grains (excluding wheat if gluten-sensitive). Probiotic-rich foods like yogurt (if tolerated) and fermented products like kimchi can also promote a healthy gut microbiome.
The Importance of Professional Guidance
Digestive health is highly individualized. Consulting a healthcare professional or registered dietitian can provide personalized recommendations based on your symptoms, lifestyle, and medical history. This is especially important when implementing elimination diets, which should be carefully managed to avoid nutritional deficiencies.
Moving Forward with Digestive Health
Digestive wellness is achievable through informed dietary choices and a holistic approach to lifestyle management. Avoiding trigger foods like high-FODMAP items, spicy dishes, and artificial sweeteners, while embracing mindful eating and stress-reduction practices, can dramatically improve quality of life. Additionally, seeking professional guidance ensures a sustainable and tailored plan for digestive health. Small, consistent changes can lead to transformative results, empowering individuals to reclaim their comfort and confidence in daily life.
Research References
Gibson, P. R., & Shepherd, S. J. (2010). Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach. Journal of Gastroenterology and Hepatology, 25(2), 252-258.
Zhang, X., et al. (2012). Capsaicin-induced esophageal hypersensitivity in GERD patients. Digestive Diseases and Sciences, 57(6), 1606-1612.
Murphy, E. A., et al. (2015). Diet-induced obesity and gut microbiota alterations. Journal of Nutritional Biochemistry, 26(10), 992-1000.
Magnuson, B. A., et al. (2016). Biological fate of low-calorie sweeteners. Regulatory Toxicology and Pharmacology, 74, 98-107.