Introduction to Modern Stress Impact
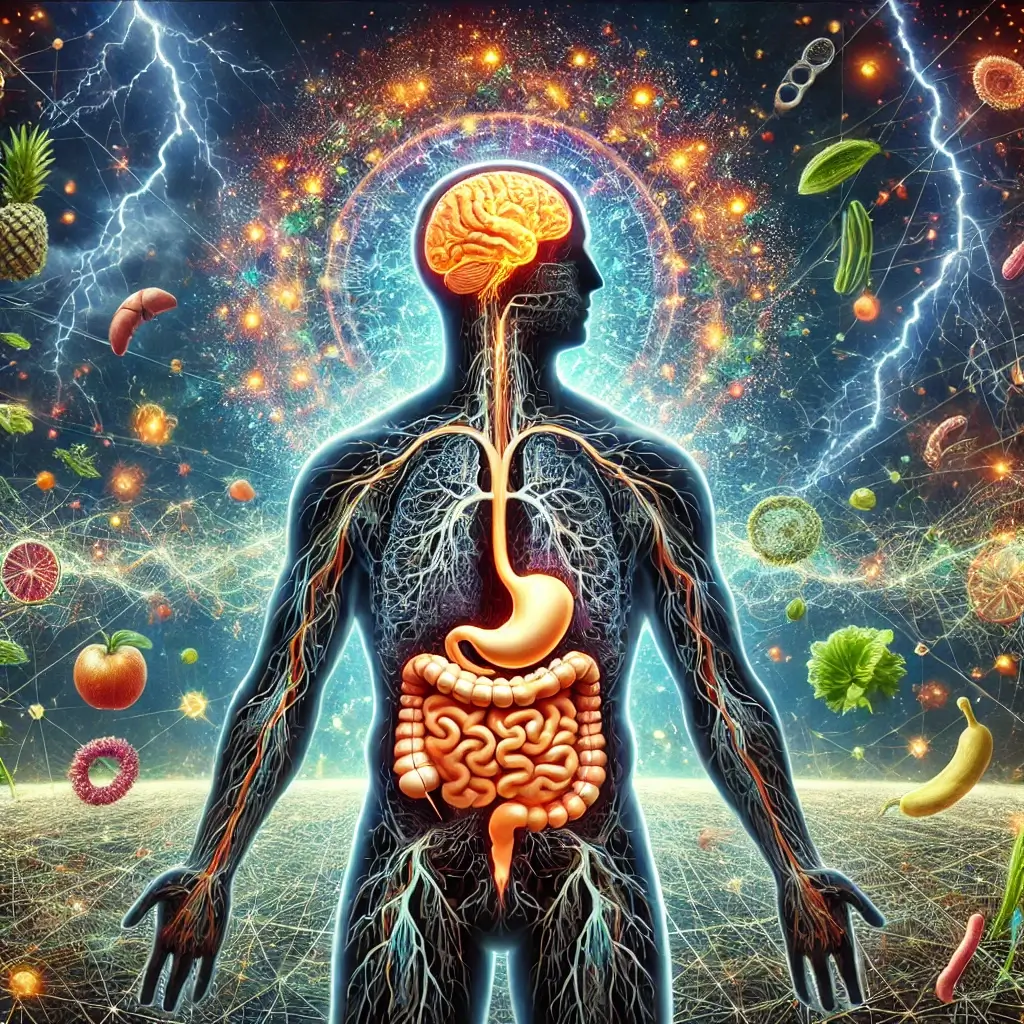
In today’s fast-paced world, stress is an almost inevitable part of life. From meeting work deadlines to managing personal responsibilities, stress often creeps into daily routines, affecting mental and physical health. While most people recognize its impact on emotional well-being, fewer understand how stress disrupts bodily systems, particularly the digestive system. This connection between the gut and brain, referred to as the “gut-brain axis,” is a sophisticated network of communication involving nerves, hormones, and microorganisms that regulate gastrointestinal function.
Long-term Effects of Stress on Digestive Health
Stress disrupts this axis, leading to various digestive issues such as bloating, constipation, diarrhea, and even chronic conditions like irritable bowel syndrome (IBS). Beyond immediate discomfort, the long-term effects of stress on gut health can lead to systemic inflammation, nutrient malabsorption, and disruptions in the gut microbiome—a collection of trillions of bacteria vital for digestion and immunity.
Research-Based Understanding
This article delves into the intricate relationship between stress and digestion, backed by medical research, and explores actionable strategies for managing stress to improve gastrointestinal health. Whether through mindfulness practices, dietary adjustments, or physical activity, understanding and addressing the root causes of stress can lead to meaningful health improvements.
Disrupted Gut Motility Impact
Stress activates the “fight-or-flight” response, diverting resources from non-essential functions, such as digestion, to immediate survival needs. Elevated levels of cortisol slow down or speed up gut motility, leading to symptoms like constipation or diarrhea. A 2017 study in Nature Reviews Gastroenterology & Hepatology highlighted how stress alters neural pathways and hormone levels, impairing the gut’s normal rhythmic contractions required for digestion (Bădărău et al., 2017).
Inflammatory Response to Stress
Chronic stress induces a low-grade inflammatory state that impacts the gut lining. Prolonged exposure to stress hormones weakens the gut’s protective barrier, allowing harmful substances to penetrate and trigger inflammation. A 2015 study in Gastroenterology linked chronic stress to elevated inflammatory markers in the gut, exacerbating conditions like IBS and ulcerative colitis (Chrousos, 2009).
Microbiome Changes Under Stress
Stress significantly affects the balance of the gut microbiome. A healthy microbiome requires a diverse population of beneficial bacteria, but chronic stress fosters the growth of harmful bacteria while reducing beneficial strains. A 2019 study published in Nature Microbiology revealed that stress-induced changes in the gut microbiota were associated with increased digestive issues, including gas, diarrhea, and discomfort (Foster et al., 2019).
Effective Stress Management Techniques
The good news is that proactive stress management can alleviate many of these digestive disturbances. Incorporating the following techniques into your daily routine can promote both mental and gut health:
Mind-Body Connection
Mindfulness techniques like meditation, yoga, and deep breathing activate the parasympathetic nervous system, counteracting the stress response. Studies have shown that regular mindfulness practice can reduce cortisol levels, improving gut motility and reducing inflammation.
Exercise Benefits
Exercise is a natural stress reliever. Activities like walking, jogging, or swimming release endorphins—hormones that elevate mood and reduce stress. Regular physical activity supports gut motility and microbial diversity.
Sleep’s Role in Gut Health
Sleep deprivation amplifies stress and disrupts digestion. Aim for 7-8 hours of uninterrupted sleep each night to help the body recover and maintain a balanced gut-brain axis.
Dietary Considerations
A diet rich in fiber, fruits, vegetables, and probiotics supports gut health by nourishing beneficial bacteria. Avoiding excessive caffeine and alcohol is equally important, as these substances can exacerbate stress and digestive issues.
Professional Health Support
If stress feels overwhelming, consider therapy or counseling. Cognitive-behavioral therapy (CBT) has shown promising results in managing stress-related digestive disorders.
Final Thoughts
The relationship between stress and digestion underscores the importance of holistic health management. Stress may be a constant in modern life, but its negative impact on the gut does not have to be. By adopting stress management techniques, individuals can improve digestive health, enhance overall well-being, and build resilience against life’s challenges. For persistent digestive issues, consulting a healthcare provider is crucial to rule out underlying conditions and develop a tailored treatment plan.
Research Citations
Bădărău, I., Walker, A. K., Hammer, H. C., & Dinan, T. G. (2017). The gut-brain axis and the nervous system in irritable bowel syndrome. Nature Reviews Gastroenterology & Hepatology, 14(12), 723-736.
Chrousos, G. P. (2009). Stress and disorders of the stress system. The New England Journal of Medicine, 360(21), 2260-2267.
Foster, J. A., McVey Neufeld, K. A., Mao, R., Gänzle, M. G., & Wachtershauser, A. (2019). Stress, strain-specific probiotics, and the gut-brain axis. Nature Microbiology.